Touchscreens seem to belong everywhere, from labs and clinics to check kiosks. But what if those “everywhere” “anywhere” surfaces are silently working against patient safety and efficacy?
Healthcare-associated infections remain a huge problem. In Europe alone, the ECDC estimates that 4.3 million patients in acute-care hospitals acquire at least one healthcare-associated infection every year. https://www.ecdc.europa.eu/en/news-events/each-year-43-million-patients-hospitals-eueea-are-affected-healthcare-associated. Given how common shared devices are in hospitals and labs, it’s worth pondering: could part of this infection risk stem from how we interact with our tech?
The Hidden Danger On Surfaces
Pathogen transmission through inert surfaces is a real and proven phenomenon. Clinical touchscreens frequently retain pathogenic bacteria. According to a study in the BMC Infectious Diseases, Methicillin-resistant Staphylococcus aureus and Acinetobacter baumannii were found on hospital computer interface surfaces. Researchers found hospital-acquired pathogens on computer keyboards and desktop screens in hospital wards, supporting that shared digital devices can act as stores for nosocomial bacteria (bacteria that cause infections in a healthcare setting) https://link.springer.com/article/10.1186/1471-2334-9-164
Furthermore, research indicates that even gloves, often regarded as the standard protective measure, can become contaminated when handling shared surfaces. Empirical evidence signals that gloved hands frequently contact multiple surfaces per care episode, spreading bacteria rather than containing it. This highlights that the hidden danger isn’t always obvious: surfaces can remain a contamination source despite standard precautions. https://pubmed.ncbi.nlm.nih.gov/26447080/
Cleaning is not enough. One simulation study modeled how public touchscreens like kiosks can contribute to infection risk. Assuming realistic cleaning rates, the simulation still calculated an infection risk of 3% per user flow. https://pubmed.ncbi.nlm.nih.gov/35333886/
Much Is On The Line
- In the U.S.A., 2 million patients acquire healthcare-associated infections every year, contributing to roughly 100.000 deaths. More people are killed by HAIs than by automobile accidents, fires, and drowning combined. Hard to believe, but true. https://effectivehealthcare.ahrq.gov/sites/default/files/infectiousdisease_hi_impact.pdf
- These infections also carry a massive financial burden, costing tens of billions per year. The cost in the U.S. ranges from 28 billion $ to 45 billion $. https://pmc.ncbi.nlm.nih.gov/articles/PMC9949640/
- For medical device and hospital teams, this is not just a hygiene challenge; it’s a patient-safety problem.
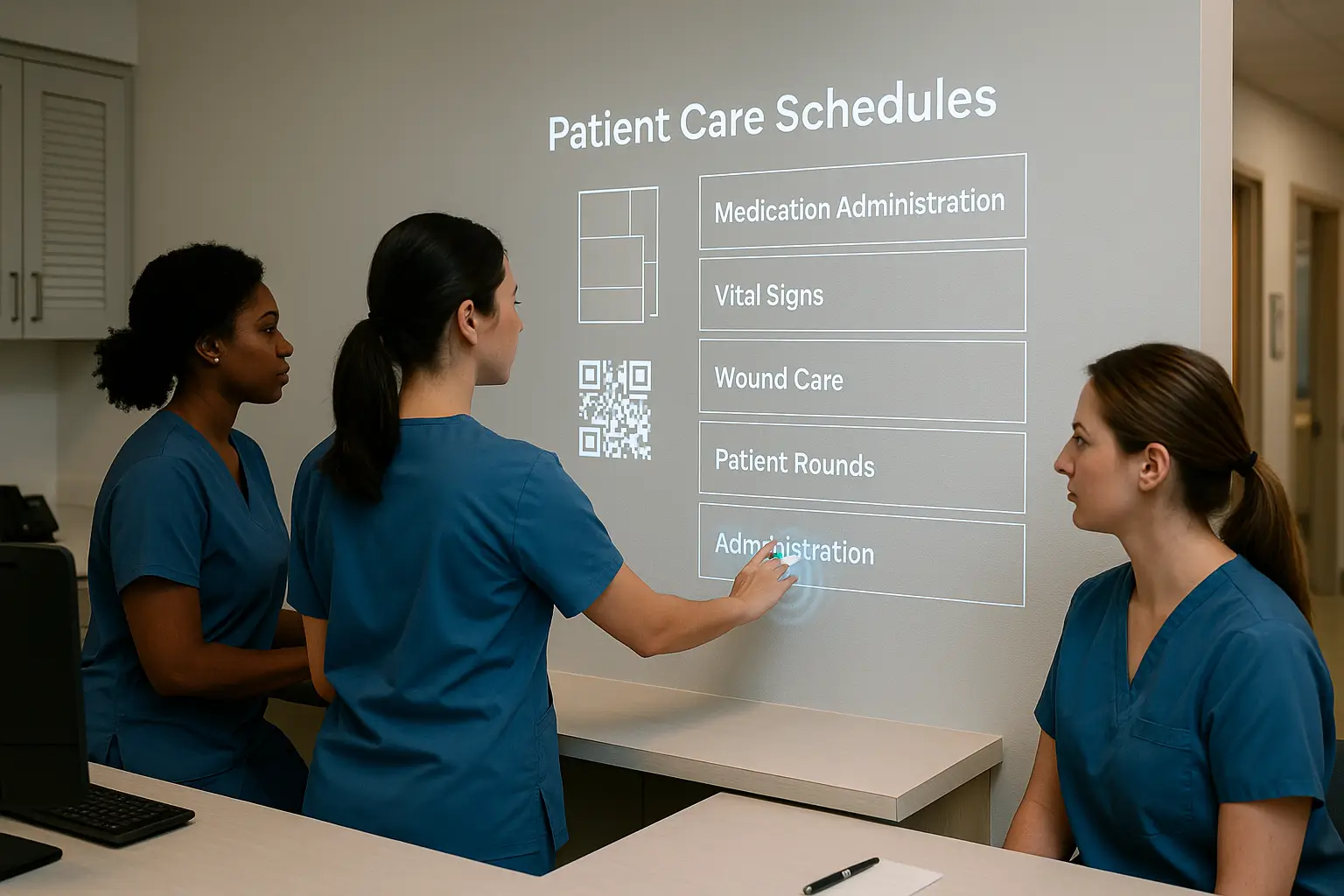
Why Touchless Tech Can Help
- Less contact, less risk. By removing or decreasing the need to touch shared digital interfaces, you reduce the chances of pathogen transmission.
- Cleaner workflow, safer, faster care. Clinicians can interact with digital protocols without pausing to disinfect, change gloves, or touch shared surfaces, freeing them to focus even more on what matters most: patients and critical decisions.
- Integrates with what you already use. The best touch-free tech can map to existing web apps, meaning you don’t need to rebuild your workflows. This saves time and avoids cognitive load.
- Scalable. If designed correctly, touchless systems can run on standard hardware, making deployment easy and feasible.
While a touchless interface is just one tool among many in improving patient care and clinician workflow, it has become essential. This technology to reduce risk is not futuristic; it’s here, and it works.
In the upcoming posts, I will dive into real-life cases. Stay tuned!
0 Comments